So, you’re starting to feel unwell. Your throat hurts, your head aches, you feel tired and you’ve developed a cough.
You’ve recently had COVID but as we now know, it’s possible to be reinfected.
But how sick will you get the second time?
While your symptoms are likely to be less severe, in some cases they can be worse. Here’s what we know so far.
After COVID, you don’t need to test for 12 weeks
Current guidelines define you as a “cleared case” for 12 weeks after ending COVID isolation. If you develop COVID-like symptoms in that 12 weeks, you don’t need to be tested.
The science behind this 12-week timeframe is evolving. The original idea was that if you have recovered from COVID, and you have a healthy immune system, you will have developed immunity against reinfection. And this will protect you for at least 12 weeks.
As case numbers in Australia increase, the reports of reinfections are also on the rise. And it’s likely reinfection is occurring sooner than we first thought.
What’s happening in our body?
In order for a person to fight off re-infection with any virus, they must have developed a protective immune response.
Two main factors decide whether a person will have a protective immune response:
1) how long a person’s immune memory lasts
2) how well that memory recognises the virus, or a slightly different virus.
Immune memory is made up of many critical parts, which each play a role in the protective army of your immunity. The biggest players in protective immunity memory are your B-cells (which mature to make antibodies) and your T-cells (which destroy virus-infected host cells).
So far, the evidence suggests immune memory for SARS-CoV-2, the virus that causes COVID, lasts for months or even years when it comes to B-cells and the antibodies they produce.
Similarly, current evidence shows the memory T-cells can last over a year.
This means that for a healthy person, immune memory for SARS-CoV-2 appears to last for a year, against reinfection with the exact same virus.
So why the reinfections?
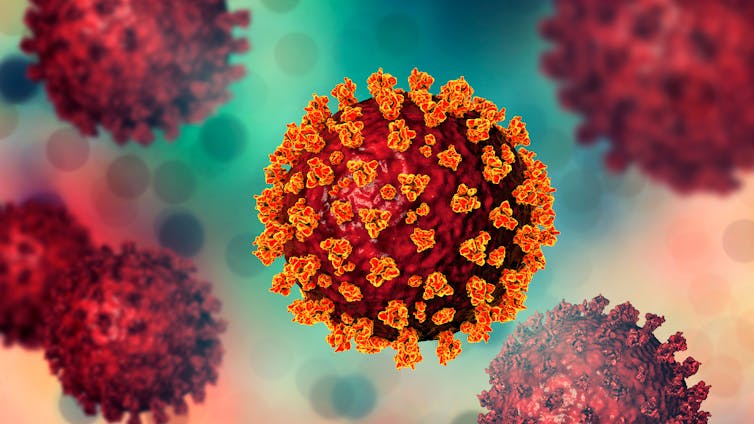
One clear explanation for reinfection is the virus is mutating. SARS-CoV-2 replicates fast and in doing so makes replication errors. We refer to these errors as mutations. Over time, the mutations accumulate and a new sub-variant is born.
Since the start of the pandemic we have seen the parental Wuhan strain mutate to Alpha, Beta, Delta and now Omicron.
The current theory is that immunity from one variant may not provide enough protection from another.
Data so far suggest the Omicron variant is better at immune escape than its predecessors. This means Omicron is “escaping” the immune memory created by SARS-CoV-2 infections from other variants such as Delta, Beta or Alpha.
Emerging data is now showing sub-variants of Omicron can also escape immunity from a previous Omicron variant. This means a person might be able to get an Omicron reinfection.
A small, yet to be peer-reviewed study from Denmark found that in unvaccinated people, reinfection with Omicron BA.2 is possible following a primary infection with Omicron BA.1. Despite this finding, the study also concluded reinfection rates were low and therefore rare.
With winter approaching and case numbers climbing, we’re also seeing the emergence of new sub-variants such as BA.4 and BA.5. Early evidence shows these new sub-variants are even better at escaping immune memory than the parental BA.1 Omicron.
What about severity?
For those who get a reinfection, disease severity appears to be milder and less likely to result in hospitalisation. This is likely because the immune memory can recognise at least part of the re-infecting virus.
However it’s difficult to measure disease severity on a population level. A systemic review of case studies found that while some second infections were milder, this was not so in all cases. Some reinfections resulted in worse outcomes, including death. (During this study period, one of the original strains, B.1, caused most primary infections, with reinfections caused by Alpha or Beta variants.)
But while Omicron appears to be causing more reinfections than other variants, there isn’t enough robust data to make firm conclusions about the severity of reinfection with Omicron or other variants.
What we know for certain is we need more data from more people to say that reinfection is less severe.
We also know from several studies that being vaccinated does provide protection from reinfection, including in previously infected people who then receive subsequent vaccines.

Another reason to get boosted
A recent study that’s yet to be peer-reviewed found immunity from Omicron BA.1 variant drops around 7.5 fold with the new Omicron BA.4 and BA.5 variants. This means the antibodies you produce from a BA.1 infection, which are able to detect and neutralise the BA.1 virus, are 7.5 times less able to recognise and neutralise BA.4 and BA.5 than BA.1.
This study also found vaccination plus natural exposure to Omicron BA.1 gave five times greater protection to Omicron BA.4 and BA.5 than the immunity from natural exposure to BA.1 alone.
Data also shows the strongest protective immunity comes from a mix of triple vaccination and natural infection.
A further study found this type of hybrid immunity protects better against both reinfection and hospitalisation than natural immunity alone, highlighting the importance of vaccination and vaccine boosters.
So the question remains: if our immune memory lasts for a year, but is too specific to recognise the new variants, will we need a new vaccine every year? Time will tell.
Lara Herrero, Research Leader in Virology and Infectious Disease, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.